A pig liver makes its way into a human
Approximately 2,000 people die every year waiting for a liver transplant. Pigs might help change that!
There are approximately 50,000 organ transplants performed every year in the United States.
Of those, about 10,000 are liver transplants.
The liver is a specialized organ that aids in digestion and produces enzymes important for removing toxic substances from our blood stream.
It also produces bile which helps to digest fatty acids and cholesterol.
The liver is the second most transplanted organ behind the kidney.
Organ transplantation is an intense and complicated surgery, but even if the surgery is successful, we still have to deal with the immune system!
We, unfortunately, can't just take an organ from one human and stick it into another because the recipient's body sees that organ as a foreign substance and the immune system treats it like an invader.
This can lead to:
Hyperacute rejection - usually caused by ABO blood typing and HLA mismatches with the body attacking the new organ in minutes to hours.
Acute rejection - this can happen after weeks to months with the recipient's T-cells attacking the donor tissue directly and B-cells making antibodies that tell other immune cells to attack the tissue.
Chronic rejection - constant bombardment from the recipient's immune system leads to a build up of organ damage.
To limit or delay these rejection scenarios, transplant recipients are matched with donors who have similar ABO and HLA profiles.
They're also placed on immunosuppressants to help prevent organ damage after transplantation.
But there aren't enough organs to go around and thousands of people die every year waiting for an organ transplant.
One solution here could be to use animal organs as human organ surrogates.
Pigs have become a popular choice since their organs are the right size and shape and function similarly to human organs.
But we have an even worse rejection problem when it comes to pigs because there's no way to type match a human to a pig!
In recent years, researchers have attempted to get around this problem by humanizing pig organs with genetic engineering to make them "look like" human organs to the immune system of the recipient.
There has been some success with this with other organs such as pig hearts (2 months) and kidneys (6 months).
However, "xenotransplantation" (when you put an organ from one animal into another) had never been done before with a liver.
That changed a few weeks ago when a brain dead recipient received a genetically modified pig liver.
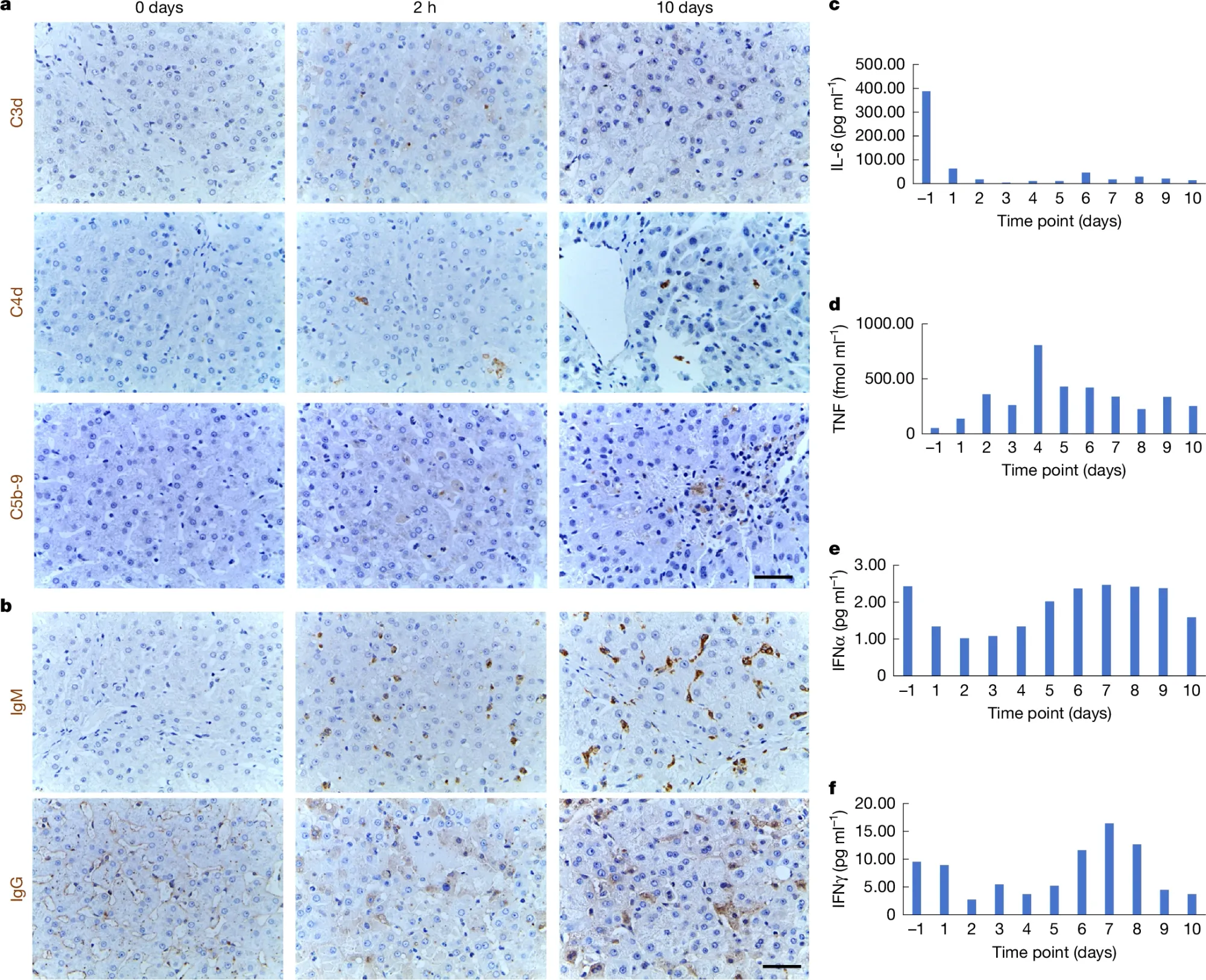
The figure above shows how the patient’s immune system responded to the new liver during the 10 day trial. a) is an immunostain (uses antibodies) of liver tissue and shows little to no deposition (brown blobs) of complement factors (C3d, C4d, C5d-9) which are hallmarks of immune activation; however, b) displays moderate staining for IgG and IgM at 10 days post-transplantation indicating that the humoral immune system may have been activated (they also saw a spike in B cells which were suppressed with rituximab) and in c-f) the major cytokines all appeared to have behaved during the 10 day window suggesting that the immune response was well controlled.
However, detecting IgG and IgM (along with the B cells) was unexpected and was not observed in their previous trials with gene edited pig livers in monkeys.
Despite this immune activation (which would eventually lead to rejection), it could be feasible to use pig livers in humans for short periods of time while they wait for a human transplant to be available.
Overall, this work provides insight into the feasibility, immunological dynamics, and technical challenges of liver xenotransplantation.
It also highlights the need for significantly more research into figuring out how to make pig organs play nice with our immune systems!
