Real-Time monitoring of hospital pathogens pays dividends
Hospital genomic surveillance of pathogens stops outbreaks, prevents deaths and saves a bunch of money.
Hospital acquired infections (HAI) are a big problem in healthcare.
Not only are they expensive to treat, but they often lead to unnecessary deaths.
The most common pathogens involved in HAI's are Clostridioides difficile, Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococci (VRE), and multidrug-resistant Gram-negatives like Klebsiella pneumoniae and Pseudomonas aeruginosa.
The challenge in detecting these deadly bugs is that HAI monitoring has traditionally been a reactive exercise where we're always playing catch up when it comes to an infection or an outbreak.
Most hospitals rely on passive surveillance to detect a rise in infections above baseline levels which then leads to an investigation after an outbreak is already in full swing.
But the tools in our molecular testing toolkits have become cheaper and higher throughput now and could allow us to be more proactive about pathogen and outbreak surveillance.
One of the options here is to perform routine environmental monitoring of a hospital and its patients using whole genome sequencing.
This allows for early detection of outbreaks and enables quicker intervention.
However, widespread adoption of WGS for these activities in the hospital setting has been hindered by cost, lack of infrastructure, and limited institutional incentives.
In response to these challenges, researchers developed the Enhanced Detection System for Healthcare-Associated Transmission (EDS-HAT).
This system integrates real-time WGS surveillance with algorithm-driven outbreak detection.
After a promising retrospective analysis of a Klebsiella outbreak in their endoscopy unit, the researchers then used the system in a two-year study that provided powerful evidence of its effectiveness:
1) They were able to detect outbreaks with as few as two positive cases
2) In 95.6% of outbreaks, interventions guided by WGS surveillance successfully halted transmission
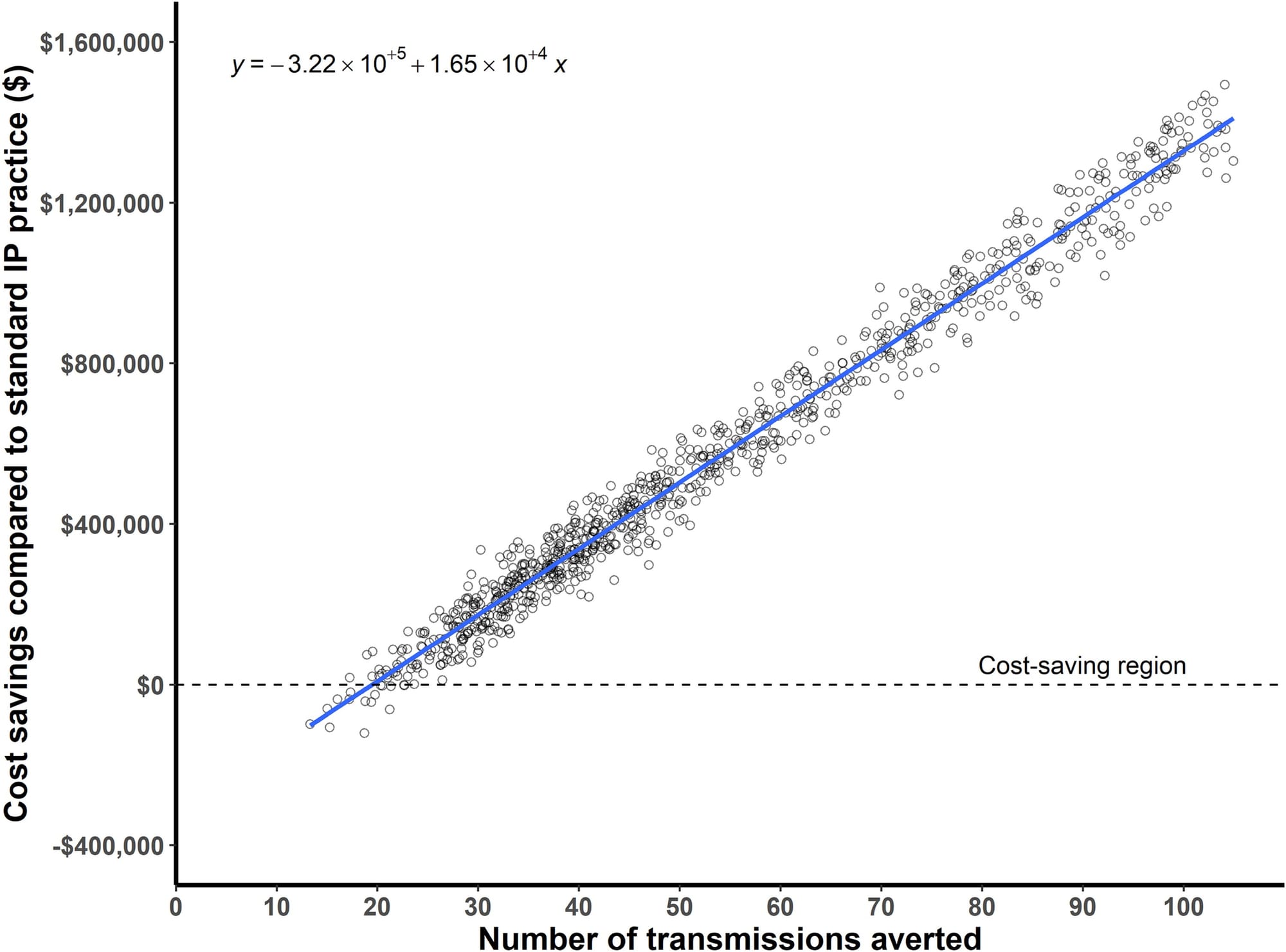
3) Real-time genomic surveillance had a net savings of $695,706, with a potential upper-bound savings reaching $1.77 million and 126 prevented infections (See figure above)
But most importantly, they estimate that 62 infections and 4.8 deaths were prevented during the study period.
This study offers powerful evidence that real-time genomic surveillance is feasible and highly effective in identifying and mitigating outbreaks.
So it goes without saying that integration of WGS-based surveillance seems like a no-brainer when it comes to hospital infection prevention and control practices.
